Exploring the Challenges and Progress of Artificial Hearts in Cardiovascular Medicine
In the intricate world of cardiac care, where the heart is seen as a complex pump, medical professionals have long sought solutions for patients suffering from severe heart failure. The scarcity of donor hearts, particularly in countries like Germany with stringent organ donation consent requirements, has led researchers to explore alternatives, including artificial hearts.
The concept of artificial hearts has been in the medical landscape for over six decades, but it wasn’t until 1982 that the first complete and permanent artificial heart was implanted in the United States. However, these early artificial hearts lacked customization, posing challenges for patients with specific needs.
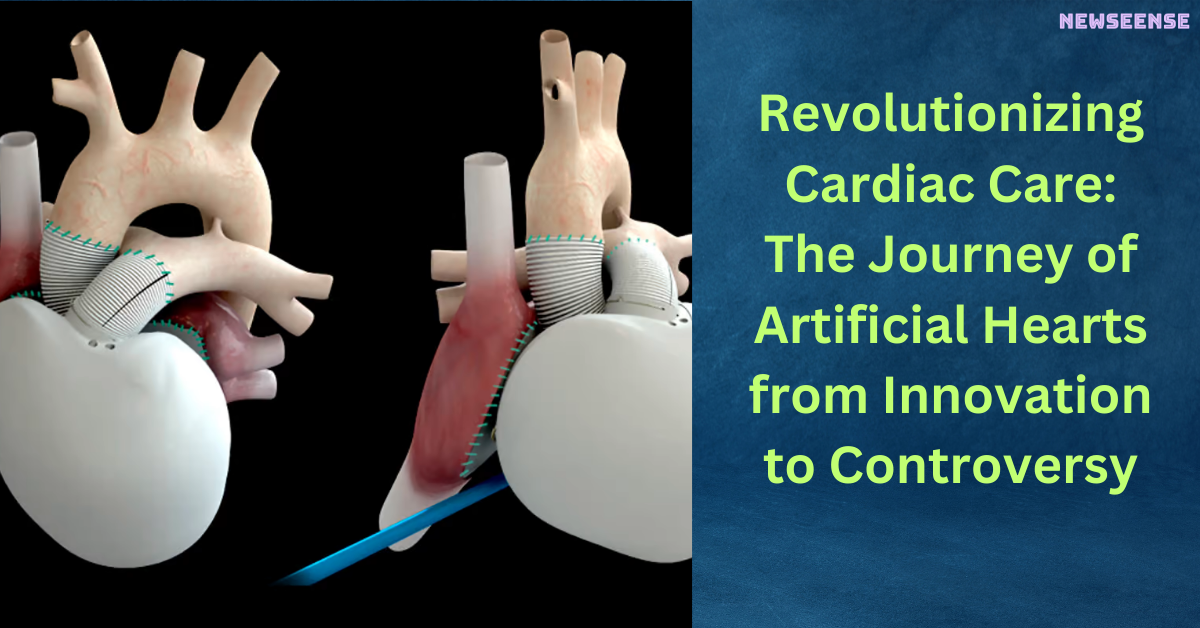
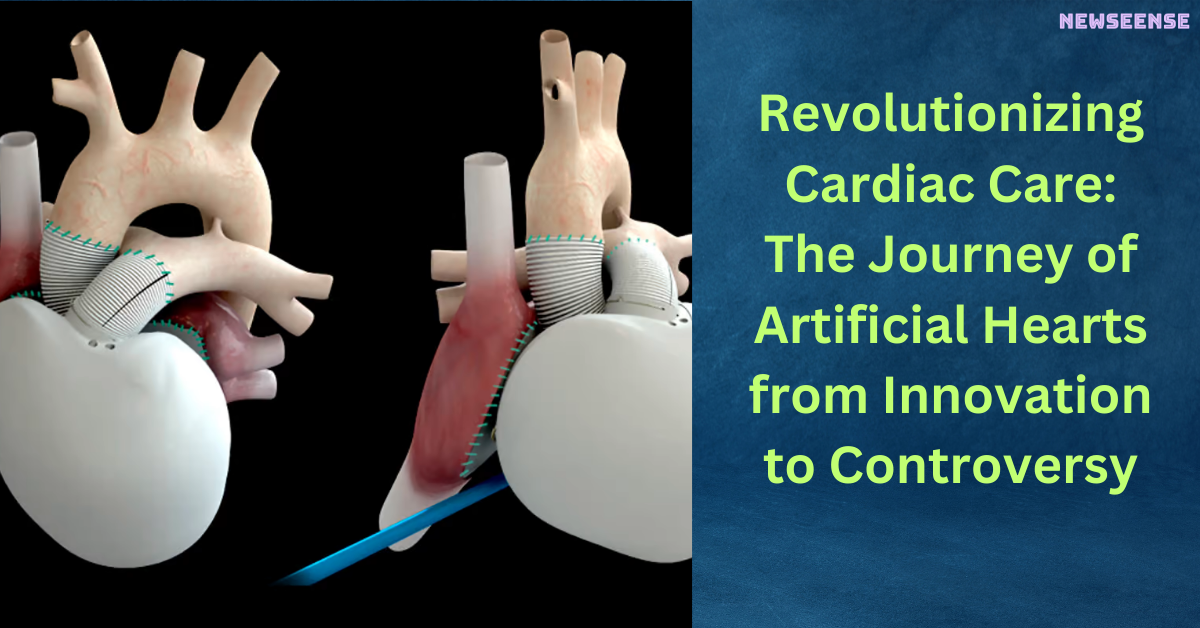
A groundbreaking development came with the Carmat heart, a creation of French heart surgeon Alain Carpentier. Unlike its predecessors, the Carmat heart was designed to adapt to the physical activity of the user, allowing for a more flexible lifestyle. This innovation marked a significant advancement, especially for patients who required a complete heart replacement.
Over the years, the Carmat heart has undergone several refinements in surface material, software, and pumps. Approximately 50 of these artificial hearts have been implanted in patients, offering an interim solution for those awaiting a donor heart. Despite its technological prowess, the Carmat heart faces challenges, including its large size, making it unsuitable for smaller chests, particularly affecting women.
Stéphane Piat, the head of Carmat, acknowledges the complexity of the artificial heart, comprising around 250 components, each susceptible to malfunction. This complexity makes the Carmat heart more vulnerable compared to other artificial hearts available. Additionally, the cost of approximately $200,000 per heart raises questions about accessibility and affordability.
The temporary nature of the Carmat heart as a solution is highlighted, with around half of the transplanted patients not surviving beyond six months. However, it’s crucial to note that these patients are often already in critical health conditions, and the artificial heart serves as a bridge while they await a donor organ.
Looking ahead, there are aspirations to move towards long-term therapy with the Carmat heart, though challenges remain, including the need for reduced size and technical improvements. The company faced setbacks in 2021 when the product was temporarily taken off the market due to quality issues.
In the broader landscape of cardiac care, researchers are exploring alternative avenues, such as genetically modified pig hearts and engineered tissues. The quest for solutions continues, raising questions about the future of artificial hearts and the potential impact of evolving technologies and attitudes toward organ donation.
This journey unfolds against the backdrop of a medical landscape striving to balance innovation, ethical considerations, and the pressing need for life-saving interventions in the field of cardiovascular medicine.
Also read: https://newseense.com/celebrating-creativity-and-credit-copyright-law-day-2024/
- BJP President JP Nadda Issues Notice to Dilip Ghosh Over Controversial Remarks on Mamata Banerjee
- Ram Charan and Kiara Advani’s ‘Jaragandi’ Song from Game Changer Released
- Pre-Match Banter: Rohit Sharma’s Flying Kiss Recreation Adds Spice to MI vs SRH Clash
- Swami Smaranananda Maharaj, President of Ramakrishna Math and Ramakrishna Mission, Passes Away at 95
- Stand-up Comedian Munawar Faruqui Breaks Silence on Social Media After Mumbai Police Detention